Understanding Angle Alpha & Angle Kappa- the finer aspects
- Subhabrata Bhattacharya

- Feb 24, 2024
- 11 min read
Updated: Apr 7, 2025
There has been a lot of talk about angle kappa and angle alpha in the past two decades. Therefore I do not want to turn this article into another write up of what is angle kappa and angle alpha. It is well known that while angle kappa is the difference between pupillary axis and visual axis, angle alpha is the difference between the optical axis and the visual axis. Thus in both, visual axis is common.
Visual axis is the line that is drawn from the fixation target to the first nodal point of eye, and thereafter from the second nodal point of eye to the fovea. However, the angles of the eye are actually theoretical. There is no instrument in ophthalmology that can accurately determine the following:
Visual axis: visual axis cannot be determined by any clinical instrument, except the synaptophore. Thus angle kappa could be measured only with the synaptophore. All other machines are approximations.
Optical axis of eye and optical axis of cornea: By definition optical axis of an artificial lens is an imaginary line that passes through the center of the two refracting surfaces(Fig1). It is also called the Principal axis. A ray of light passing through this surface remains undeviated as it always passes perpendicular to surfaces.
However, in the eye the geometric center of the cornea (center of limbus) may not be the optical center of cornea. Even if we assume that geometric center is the optical center, it will still be difficult to exactly locate the geometric center of the cornea, as cornea is not a perfect sphere. Thus the optical axis of cornea is often substituted by a line perpendicular to the cornea plane and joining the center of the pupil (Fig2). The center of the pupil in itself is not constant, right? It varies with different lighting condition, as much as with age. So yes, there is a lot of assumption and simplification.
That was about optical axis of cornea. The optical axis of eye will be the line that is perpendicular to the plane of cornea and intersects the center of pupil (optical axis of cornea) that extends and goes through the nodal point of eye and reach the retina. There are again several assumptions here. Even if we theoretically locate the optical axis of the human eye in this way, such a line does not reach the fovea. Thus this theoretical line that travels through the optical axis of cornea, nodal points, reach the retina slightly nasal to the fovea. In other words, the fovea lies temporal to the assumed optical axis of eye.
All cardinal points like the Principal Point, nodal points, centre of rotation of eye, primary and secondary focal points will then fall on this line. However, in reality such points do not coincide in the eye.
For multifocal IOLs centration plays a critical part. The surgeon may ask the patient to look at the coaxial light of the microscope in the operation theatre, and align the purkinje reflex from lens (P3) to that of cornea(P1). However, if major decentrations are there, the lens may take its natural position with capsular contraction in the capsular bag.
Thus if optical axis of eye is a theoretical concept, angle alpha, which is the difference between the optical axis and visual axis is difficult to measure in a clinical set up. Angle alpha is determined at the nodal point of eye. The primary nodal point is 7.039 mm posterior to corneal vertex and the secondary is 7.321 (1). Angle alpha as well as angle kappa could be measured by a Synoptophore which most practices do not have, today.
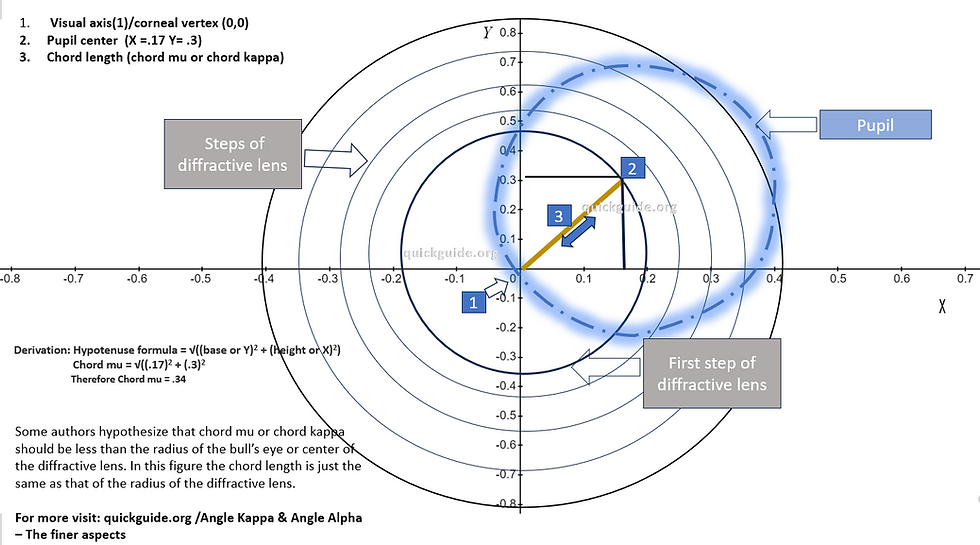
Chord mu and CW-Chord (Fig 3 highlighted in yellow) are alternative terminologies that have been proposed to work around the difficulty of obtaining angles alpha and kappa in a practice. The optical biometers report CHORD MU, as defined by Dan Chang and George Waring IV, which is the chord (straight line that joins end of two points) from the Vertex Normal Light Reflex (Purkinje 1) and the center of the pupil. The angle is actually Kappa. Chord mu is a distance between Purkinje 1 (light that reflex back from anterior cornea) and the pupil center, and are images at the pupillary plane, 4.0 mm posterior to the corneal vertex (and not at the corneal plane). Chord mu is reported on the IOL Master and LenStar as Px, Pcx and Py, Pcy. They are chords/distances and not angles. One must know all of the dimensions of the eye to determine the equivalent angle and the same chord gives different angles for different eye. In text books the nominal values of 1 mm = 7.5 degrees = 15 Prism diopters, but these are just averages, so Chord Mu is used directly(2).
Thus chords are in millimeters (because they signify distances) and not in angles, and is referred to as pupil barycenter (in Lenstar) for an equivalent of angle kappa and Iris barycenter for an equivalent of angle alpha. In the below the Ix and Iy signify the distance of between the coaxially sighted light reflex and the limbal centre. The CW chord below is the value of the displacement calculated as per Pythagoras theorem as the barycentric difference of the coaxially sighted light reflex at the pupillay plane (regarded as visual axis) from the centre of the pupil (4). Thus both parameters are showing decentrations on the horizontal and vertical plane, but not the lateral tilt in angles.
A brief synopsis of how angle kappa or angle alpha is derived in different instruments:
Orbscan II - Calculates angle kappa by measuring the distance between reflection of the pacido disc from cornea and the center of the pupil (3).
Pentacam - Displays in terms of XY- cartesian coordinates, between corneal vertex(highest elevated point of cornea) and pupil center (3).
IOL Master - Measures chord mu as equivalent to kappa (Chang and Warring Chord). Distance between Purkinje reflex of coaxial light source and apparent pupil center.
Lenstar - Provides pupil and iris barycenter as equivalent to kappa and alpha respectively. The pupil barycenter is in terms of XY cartesian coordinates between the coxially sighted light reflex and pupil center. The iris barycenter is also in terms of XY coordinates between the limbal center and coaxially sighted subject light reflex/corneal vertex (P1)
If you have an optical biometry machine, that provides values in terms of XY cartesian coordinates only and does not display chord mu, and wondering how to calculate the chord length (chord kappa/chord mu or chord alpha) then you must apply the Pythogorus theorem to derive the pupil and iris barycenter distances(Fig 5). The chord length can be obtained by the square root of the sum of squares of the x and y coordinates. The resultant value is the chord mu or the chord kappa. Chord alpha calculation is no different. My own calculator in the Biometry Validation Tool (Biometry section) does that for you.(https://www.quickguide.org/post/biometry-validation-tool ).
Alternatively, you can roughly calculate by adding the X and Y values ignoring the negative and positive sign ( do not cancel a - with a + as these are displacements and signs should be ignored to get the magnitude of chord distance)
Corneal magnification affects chord mu, or chord alpha values (5). According to some studies chord mu values with IOL Master 700 differed from that of Pentacam HR. The IOL Master and other optical biometry machines may measure the distance of Purkinje reflex (P1) from the apparent pupil center seen on the cornea(apparent chord mu on the corneal plane). There is always an element of magnification. The Pentacam may provide the actual chord mu, which is the distance between the actual pupil center (sans corneal magnification because it is at the pupil plane) and the corneal vertex.
When you do not have optical biometry or a biometry machine that provides you an understanding of decentration in eye:
Implanting a diffractive multifocal IOL needs not only a proper biometry, but also a careful evaluation of the decentration of eye. If you do not have optical biometry, or any instrument that allows you to determine the decentration of eye, you could do a humble corneal Hirschberg test. Hirchberg test, also known as the corneal light reflex test, is an objective test that helps you understand the relative decentration, or even squint in the eye. It uses the 1st Purkinje reflex from cornea to understand the alignment of the eye by shinning a torch light on to the eye. A light thrown at the patient's eye sitting at a distance of approximately 50 cm, is reflected back to the examiner eye who places his eyes just behind the torch light. The torch light should be algned to the midline of the nose. The degree of misalignment of the eye can be determined by the decentration of the light reflex.
If the light reflex is centred around the pupil, then orthoposition or normal alignment is noticed. No major decentration is there in such patients.
If the relex is on the margin of the pupil, that would signify esotropia or exotropia depending on the whether the light reflex is on the temporal or nasal side.
The thumb rule is that for every 1mm of misalignment would correspond to approximately 7 degree of deviation (or 15 prism diopters). A caveat here is that the fovea is slightly temporal to the optical axis. Because the field of view is opposite to the retinal nerve fibre layers the reflex back from the fovea is centred slightly nasally on the cornea. So most patients will have the light reflex shinning from the torch centered on the pupil, but slightly nasally (positive but normal angle kappa).
Bull's eye (centre of diffractive element) and angle kappa or alpha -
It has been commonly known that the higher the central radius of the diffractive profile, that is the centre of the diffractive element or bull's eye, the more forgiving is the diffractive multifocal IOL to decentration. It has been often pointed out that the radius of the centre of diffractive element should be no less than the chord mu or chord alpha of the patient (Fig8).
The center of the diffractive element cannot be increased arbitrarily. It's width is determined by the add power that is designed in the bifocal or trifocal diffractive lens. The add power is adjusted by varying the width of the diffractive steps or rings. As the zone width is increased the add power is decreased (6). The equation that governs this relation is(8) :
Where i is the step or ring number, λ is the design wavelenth of light, Dadd is the add power of the lens, r is the radius of the ring/step. Thus if you are calculating the diameter of the first diffractive ring, the value of (2i-1) is 1. Therefore the equation stands as λ*1000/add.
Taking the Restor +4 add power lens the radius will be .375 mm. Here are the steps to calculate
convert wavelenth of light to mm : 550 nm of light is equal to .00055 mm.
Convert add power to mm :4D =25 cm = 250 mm ( 1D = 1000mm)
Multiply .00055 with 250 mm and take the root of the product
therefore r is .37. Diameter will be 2 times the radius .741
Remember the value of this diameter will change if the wavelenth of light is changed. Conceptual only.
Let us do this for the ReSTOR +2.5 and PanOptix taking wavelength of light 550 nm (conceptual only).
ReSTOR +2.5 with 550 nm of light
Convert wavelenth of light to mm : 550 nm of light is equal to .00055 mm
Convert add power to mm : 2.5 D = 40 cm = 400 mm (1D = 1000 mm)
Multiply .00055 with 400 mm and take the root of the product
Therefore r is .469. Diameter will be 2 times the radius .938mm (conceptual only)
Calculating the diameter of the bull's eye zone of trifocal IOLs that dedicate light to the intermediate (not distance):
The central bull's eye zone of PanOptix is said to be approximately 1.164 mm (9). The PanOptix dedicates light through this region to the intermediate and not the distance. How will the above calculation of the bull's eye be worked upon. For the enthusiasts, below is the calculation of how you can arrive at the bull's eye diameter of the PanOptix or any trifocal IOL that has the central bull's eye dedicated to intermediate.
· Example: PanOptix bull’s eye is dedicated to intermediate.
· The near add power of PanOptix is 3.25 dioptre. Take half of 3.25 dioptre 3.25/2= 1.625 dioptre (this could be the power of the intermediate zone in PanOptix)
· Convert the 1.625 dioptre add power to mm: 615.38 mm.
· Convert the wavelength of light to mm: .00055 mm (assuming a 550 nm of wavelength is used)
· Multiply .00055 as wavelength of light with focal length of 615.38 and take the root = .581 mm
Therefore, radius of PanOptix is .581 mm. Diameter is two times the radius, 1.16
Here is a simple calculator to help you know the diameter of central diffractive ring/bull's eye when you input the add power of the lens and the wavelenth of light. Be careful to know if the central bull's eye is dedicated to distance or the intermediate. Accordingly you can use one of the two calculators in the spreadsheet below
Thus, since the add power of the lens is directly linked to the diameter of the bull's eye, a careful choice has to be made between the two. Lenses like the Symphony (J&J) have a very high bull's eye, at the cost of a very low add power (the Symphony was marketed as an EDOF lens), while the ReSTOR +4 had a lower bull's eye (.7mm) as its add power was high. Between the two lenses is the ReSTOR +2.5 with a central bull's eye of .938mm.
In a peer reviewed clinical study (7), the impact of decentration on the Far and Near MTF was studied with regard to four different multifocal IOL models consisting of two diffractive and two refractive models. For the ReSTOR +4 lens, the near MTF detoriorated with increasing degrees of decentration, but the far MTF improved. This could be because of the design of ReSTOR +4, wherein the outer refractive zone is exposed more with an increasing degree of decentration at a given aperture size. Interesting to note here is that the ReSTOR bull's eye perhaps would be the smallest (.7mm), thus proving that there may be other factors at play that counter balance the smaller bull's eye of ReSTOR and its effect on vision in case of decentration (Fig 7).
In a study by Marques and co-authors published in 2024 (10), angle kappa was associated with post operative refractive surprise. In a study involving 67 patients, the authors concluded that a large angle κappa may reduce the predictability of IOL power calculation. The authors hypothesize that this may be due to the following facts: (1) by reducing the accuracy of keratometry readings and (2) by changing biometric length measurements as these are taken “diagonally” relatively to what formulas are design to use. The authors observed that nasal deviation of the visual axis in relation to the pupil was associated with higher absolute error. The study however involved extreme axial length eyes.
-------------------------------------------------------------------------------------------------------------------------
(1) Negative dysphotopsia: Causes and rationale for preventation and treatment: Jack T Holladay, Michael J Simpson http://dx.doi.org/10.1016/j.jcrs.2016.11.049
(2) Personal communication with Jack T Holladay, 2024
(3) Measurement of angle kappa and centration in refractive surgery: Choul Yong Parka, Sei Yeul Ohb, and Roy S. Chuck, Curr Opin Ophthalmol 2012, 23:269–275
DOI:10.1097/ICU.0b013e3283543c41
(4) Chang DH, Waring GO. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol. 2014;158:863–874.
(5) Evaluating Changes in Apparent Chord Mu after Pharmacological Pupil Dilatation:May 2023 Ophthalmic Research 66(1):1 DOI:10.1159/000530905
(6) Cohen AL. Diffractive bifocal lens designs. Optom Vis Sci 1993; 70: 461-468.
(7) Mitsutaka Soda; Shigeo Yaguchi. Effect of Decentration on the Optical Performance in Multifocal Intraocular Lenses, Ophthalmologica (2012) 227 (4): 197–204.
(8) Energy distribution between Near and distant images in apodized diffractive multifocal intra ocular lens. Fidel Vega and co authors: https://doi.org/10.1167/iovs.10-7123
(10) Marques, João Heitor MD, MSc; Baptista, Pedro Manuel MD, MSc; Ribeiro, Bruno MD, MSc; Menéres, Pedro MD; Beirão, João Melo MD, PhD; Intraocular lens power calculation: angle κ and ocular biomechanics; Journal of Cataract & Refractive Surgery 50(4):p 345-351, April 2024. | DOI: 10.1097/j.jcrs.0000000000001362