Pupil Test - A Key Element in Multifocal IOL Candidacy
- Subhabrata Bhattacharya

- Nov 27, 2018
- 7 min read
Updated: Nov 12, 2023
Understanding the pupil is very important to determine the candidacy of a patient for multifocal IOL. This is because the pupil often gives us an understanding of a bigger problem behind. It is therefore important to determine the normal physiologic behaviour of the pupil before implanting a multifocal IOL in a patient.
Observing pupil shape, location, and size.
A normal patient’s pupil should be round, symmetrical, and centered within the iris. The red reflex provided when viewing through the direct ophthalmoscope can be helpful when comparing the two eyes. Non-round pupillary shape can occur as a result of a surgical complication, posterior synechia from intraocular inflammation, or iris atrophy from age, ischemia, inflammation, or trauma.
Other gross observations for abnormalities could include evidence of corectopia (displaced pupil), polycoria (multiple pupils), leukocoria (white pupil, which can be an ominous sign of a serious ocular form of cancer known as retinoblastoma), or iris heterochromia (difference in iris colors between the two eyes). Although pupil testing provides gross observations in these areas, the slit lamp can be used to examine the pupil and iris in more detail.
Measurement of pupil size
Measurement of pupil size should occur under normal lighting conditions to the nearest 0.5 mm using a millimeter ruler or pupillary gauge while the patient fixates on a distant, non-accommodative target . To avoid stimulating the accommodative response and consequential constriction, the ruler should be held away from the visual axis of the patient. Under normal illumination, the average adult’s pupil size measures around 3.5 mm but can widely vary anywhere between 2 mm to 5 mm . Pupil size decreases as one ages due to senile miosis. Pupils should be within 1 mm in size of each other. Any difference in pupil size between the two eyes is known as anisocoria. Physiological anisocoria occurs in about 25 percent of patients, but the difference should not be more than 1 mm, otherwise it could be termed as pathological anisocoria. Pathological anisocoria could be associated with an abnormal dilatation or constriction of pupil.
Pupillary reflex
The reaction of the pupil to either light, accommodation or psychosensory stimulus is called the pupillary reflex. The pupil reacts to light stimulus. When light is thrown to one eye, not only that the pupil constricts in that eye (direct pupillary reflex), but also the other eye (on which light is not thrown) constricts (consensual Light reflex). In this article we will deep dive on this phenomenon, and understand the pupillary light reflex pathway, and what can be inferred when such reaction is not present.
Before we go into pupillary light reflex, a brief word on the two other reflex of pupil - accommodative and psychosensory reflex. The pupil constricts when we see a near object, like reading a book (near reflex of pupil). Conversely, the pupil dilates when we see a distant object. The amount to which the pupil constricts when we view a near object or dilates when we see a distant object differ from patient to patient, and between people of different races.
On the other hand, the dilation of pupil may also occur on psychic or sensory stimulus and therefore called psychosensory reflex. While the accommodative and light reflex cause the pupil to constrict, the psychosensory reflex cause the pupil to dilate.
Pupillary reaction to light

The pupillary light response consists of both an afferent (optic nerve, CN II) and efferent (oculomotor nerve, CN III) pathway. Under normal conditions, when light is shone into one eye, it will not only cause a direct response of pupil in that eye to constrict, but also a consensual response of the opposite eye to also constrict. When observing a pupil’s direct and consensual responses to light, the set-up should be dim room illumination (not dark) with the patient fixating on a distant non-accommodative target. Standing off to one side, the clinician should direct the light into the right eye and hold for two to four seconds. Make sure the light is pointed directly into the pupil—avoid holding the light too low because you do not want it directed at the patient’s cheek and watch for stray light entering the opposite eye.
The Light reflex pathway
Why does the light shown in one eye, leads to the constriction of pupil in the other eye? To answer this, an understanding of the light reflex pathway may be helpful.
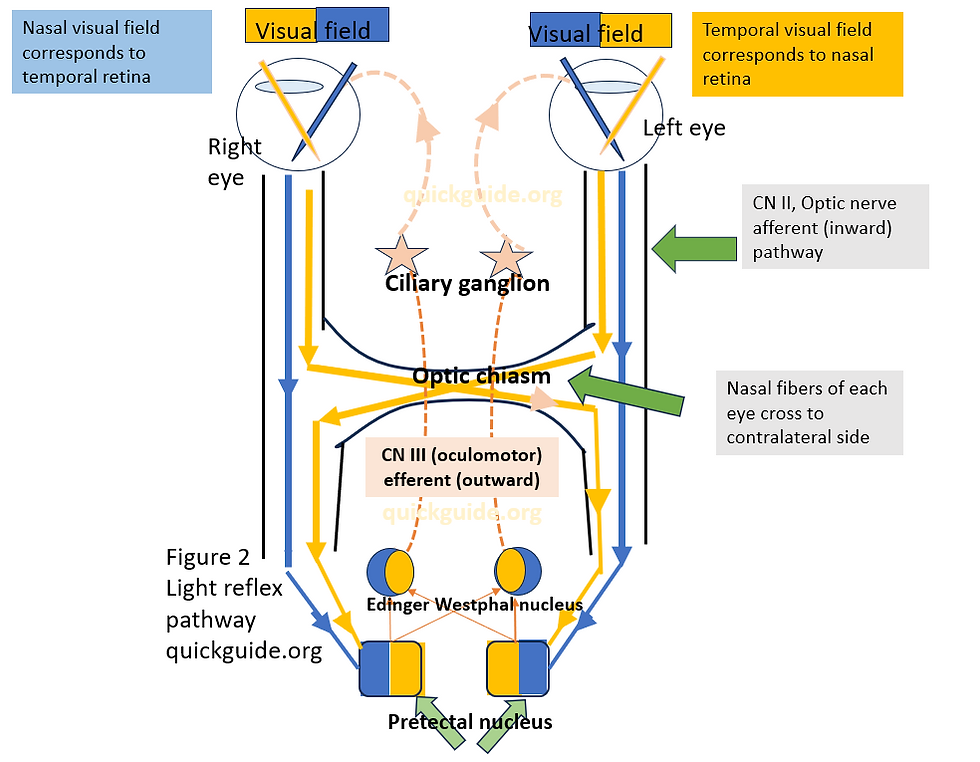
The light reflex pathway is different from the visual pathway, in the sense that the light reflex pathway avoid the lateral geniculate nucleus. To start with, the visual field of each eye is in the opposite side of the retina. In the figure 2, the two halves of each eye visual field is marked in blue and yellow. The nasal side of the visual field corresponds to the temporal side of the retina, while the temporal side of the visual field corresponds to the nasal side of the retina. Thus for the right eye, the yellow and blue colors mark the temporal and nasal side of the visual field in Fig 2. These will connect to the nasal side and temporal side of the retina (follow the arrow in figure 2 from the visual field to its corresponding side on the retina)
When we shine the light, say in the right eye, the optic nerve will pick this up. Nerves in the temporal as well as the nasal side of the left eye travels along the optic nerve ( that is the second cranial nerve). The temporal retinal nerve are marked in blue while the nasal side retinal nerve layers are marked in yellow ( right eye). They travel till the optic chiasm, where the temporal nerve fibers (blue) follow an ipsilateral path, that is, they travel past the optic chiasm on the same side and do not cross to the contralateral or other side. The nasal side nerve fiber layers (yellow) however cross the contralateral or other side of the optic chiasm. Thereafter, both the temporal and nasal side nerve fiber layers reach the Pretectal nucleus on either side. This is same for the other eye. Thus both the pretectal nucleus in the mid brain receives information from not only the same side (temporal) nerve fibers, but the other side nasal nerve fibers. The pretectal nucleus on both sides is connected to the Edinger Westphal nucleus of both sides. Thus each of the two Edinger Westphal nucleus gets information from the temporal and nasal nerve fibers of both eyes. This is the afferent (inward) path of the pupillary light reflex. In a simple language, by afferent path we mean the inward relay of information in the body.
As each of the pretectal nucleus and Edinger Westphal nucleus receives information from both sides of eye (in this case remember the light is shown on the right eye) it will now relay this information and direct the pupil of both eye to constrict. How does it do that? Herein starts the efferent (outward) pupillary pathway. The Edinger Westphal nucleus will direct the pupil of both eyes to constrict. This information is relayed through the third cranial nerve (CN III) to the ciliary ganglion cells. With the help of the ciliary ganglion cells, the sphincter pupillary muscles of the iris would get command to constrict.
As light is shown in one eye, the direct and consensual light reflex occurs because of the pupillary light reflex pathway that is connected to the Edinger Westphal nucleus of both sides of the eye, which in turn through the third cranial nerve directs the sphincter muscles of both pupil to constrict.
Pupil evaluation for multifocal IOL patient selection
A careful evaluation of the pupil is an important consideration in evaluating the candidacy of a patient for presbyopia correcting IOL. If a consensual light reflex is absent for a patient, it may be because of a lesion present in the third cranial nerve (oculomotor nerve) related to the other eye. This inhibits the patient's other eye to get light stimulus from eye that is directed to the torch light.

Again, if light is shown in the left eye, and there is an atrophy or lesion in the second cranial nerve of the left eye (Figure 3), then there will be no direct light reflex in left eye, and no consensual light reflex in the right eye. However, if light is shown in the right eye, then there will be direct light reflex in the right eye as well as consensual light reflex in left eye. This is because there is no such lesion in the second cranial nerve of right eye (afferent pathway of right eye) and no lesion present in the third cranial nerve of left eye (efferent pathway).

If a lesion is present in the third cranial nerve of right eye (as shown in Figure 4 with red arrow and box), this will lead to absence of direct pupillary reflex of the right eye, but there will be consensual light reflex in the left eye. However, the right eye will have no consensual light reflex also as there is a lesion in the oculomotor nerve ( third cranial nerve).

Swinging flashlight test The purpose of the swinging flashlight test is to compare the strength of the direct pupillary response with that of the consensual response in the same eye. In a dark room, with the patient fixating on a non-accommodative distant target, the light beam is directed into the right eye and held for two to four seconds, then quickly moved to the left eye and held for two to four seconds. This process should be repeated for at least three to four cycles. When moving the light between the eyes, use a slight u-shaped motion, making sure to avoid the transilluminator crossing the patient’s visual axis, which may stimulate accommodation.
It is critical that the magnitude and duration of the light be kept the same for each eye. Observe the response of the pupil receiving the light, the degree or rapidity of pupillary escape, and the response and size of the pupil not receiving the light. A normal patient should show equal direct responses between the two eyes. In addition, the rate and amount of constriction should be the same for both pupils.
When the consensual response is greater than the direct response in the affected eye, then the patient is classified as having a relative afferent pupillary defect (RAPD, APD, Marcus-Gunn pupil), signifying unilateral or asymmetric damage to the anterior visual pathway. Thus the patient may have an atrophy or an optic nerve damage in the second cranial nerve before the optic chiasm. Thus in a relative afferent pupillary defect, the consensual reflex is more than the direct light reflex due to the presence of lesions in the optic nerve pathway of the affected eye.
A thorough evaluation of the pupil is important for determining the candidacy of the patient for multifocal IOLs for cataract surgery. The aim of the article is to not guide in treatment of such patients, but how we can identify anomalies in pupillary reaction so that little clues can be picked up to avoid a bad outcome with presbyopia correcting IOL. For a thorough evaluation of patient's candidacy you may refer to the chart for complete anterior segment evaluation by clicking on the link below:
----------------------------------------------------------------------------------------------------------------------------------------





