The Science Behind Keratometry & the concept of Keratometry index (K Index)
- Subhabrata Bhattacharya

- Mar 20, 2019
- 8 min read
Updated: Dec 16, 2025
Recently I was involved in a discussion on different makes of Keratometers by different companies. Many of the participants voiced their concern on the difference of reading between many different Keratometers, leading to a confusion as to which data to be relied on. On a separate article named " What to do when your K readings are different from different Keratometers " (https://www.quickguide.org/post/what-to-do-when-your-keratometry-readings-are-different-from-different-keratometers ) this issue has been addressed. This article however would concentrate on why do different Keratometers, optical or otherwise, fail to have consistency amongst the readings. In answering so, I would also take you briefly through the science behind the calculation of the modern optical biometers.
As we understand, different Keratometry devices read different rings of the cornea. While the manual Keratometers would typically measure at central 3.0 to 3.2 mm of cornea, the optical Biometry machines like IOL Master would measure 2.5 mm of the cornea (IOL Master 500). The Lenstar measures two separate rings of 1.65 and 2.3 mm of cornea approximately. The Verion from Alcon measures around central part of .8 to 1.2 mm of the cornea while it takes the axis from a broader ring beyond this area. As you can see, none of the keratometry devices measure one common area of the cornea, and it varies between the make of the devices. One big reason for the differences of the readings is heterogeneity of measurement areas.
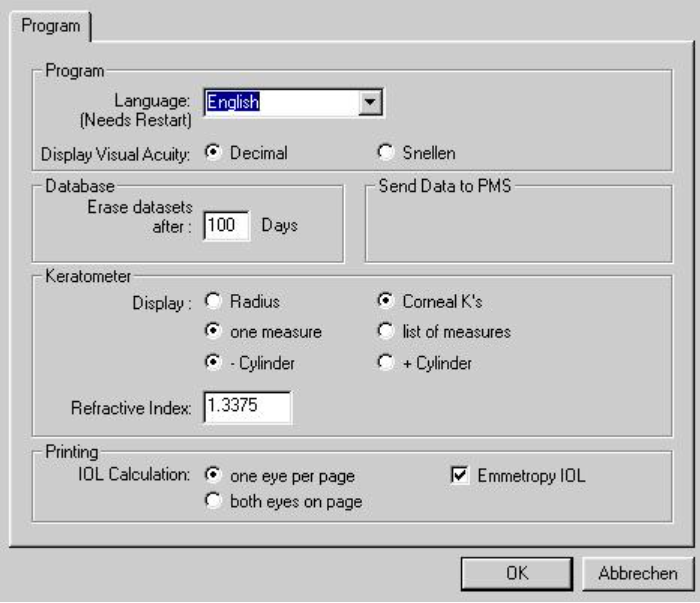
Another factor in the difference of the reading is the Keratometry Index ( K Index ) employed by the devices. A point to be noted here is that Keratometry does not measure the cornea in diopters directly. It measures the radius of curvature of the cornea (roc) in millimeters (mm), which is then converted back to diopters through a formula ( D=n-1/r ) where n is the Keratometry Index, r is the radius of cornea, and 1 is the refractive index of air. The European and US make devices do not have the same K Index. This would therefore lead to further differences in the final K reading between the devices. Generally, the Keratometry Index (K index) of 1.332 is normally used in Europe, while in USA a K Index of 1.3375 is used. Depending upon the keratometry device that you use, K Index could be as varied as 1.3315, 1.336, 1.3375 and 1.338.
Since in keratometry we first measure the radius of curvature (roc) of the cornea, the Keratometry Index or K Index helps to convert the radius of curvature to dioptric value of the cornea. If the Keratoemtry Index of two machines are different, say for instance one uses 1.3375 and the other 1.332, then needless to say, the final power of cornea will be different. Thus to match the Keratometry readings between two devices, it is essential to ensure that the K Index of both Keratometers are the same. Otherwise, while radius of curvature will be the same (assuming both keratometers measure the same area of corneal ring) dioptric power of the cornea will be different. That being said, the keratometry index of 1.3375 is widely used today.
Have a look at the table below to appreciate how the K index may influence radius of curvature of 7.50 mm conversion back to diopters:

As you can see in the above table, between a K index of 1.332 and 1.3375, a radius of curvature of 7.50 mm of cornea may vary upto .70 diopters. The two K index of 1.3375 and 1.332 are the most common K index commonly used by keratometers, but some keratometers also use other values.
It is important to state that the common K Index used by devices like IOL Master and Lenstar is 1.3375. Why did they choose a K Index of 1.3375?
This is because taking a Gullstrand ratio of anterior to posterior cornea as .883, that is the radius of curvature of cornea being 7.7 and 6.8 mm (6.8/7.7) of anterior and posterior cornea, the K Index of cornea as 1.3375 closely approximates the average power of the cornea.
So long we have been discussing why two keratometry readings of same patient from two different keratometers may be different. Now let us look at the issue from TORIC calculation point of view. There are many TORIC online calculators, like that of the HOYA, ALCON, or the J&J calculators. These toric calculators provide us the toric model, intended axis of placement and the potential residual astigmatism likely for the patient. While we input the K readings in diopters into such online calculators, it is essential to specify the K index of the keratometry device from where the corneal reading is being sourced. Otherwise, there could be a potential mismatch between the K index used by the calculator and the K index of the keratometry device. This can lead to sub optimal patient outcomes. Below is a picture of the HOYA online calculator, which gives an option of providing the K index of the keratometry device for the corneal readings.

Where such option is not available, for example in Alcon TORIC calculator (below image), it is important to input values only in radius of curvature, to avoid a potential mismatch in K index of the online calculator and the keratometry device.

An important point to note, most IOL formula, especially the two variable formulae with the exception of Haigis, assume that the Keratometry has been done with a device having a K index of 1.3375. Thus SRK T, Holladay 1, Hoffer Q assumes that the keratometry readings are input from a keratometry device which uses K index of 1.3375. The starting point of these formulas is to convert the anterior corneal power to net optical corneal power by using a lower k index like 1.333 (4/3) used by Binkhorst or 1.3315 used by Olsen.
An example of standard method used by IOL calculation formulae of converting the anterior keratometric power (Kk) to the net optical power of the cornea (Ko) is shown below (source Jack Holladay):

Here 4/3 is is the net corneal index of refraction (4/3= 1.333 used by Binkhorst). SRK T uses the corneal refractive index of 1.333 like that of Binkhorst and Holladay 1 *.
Thus if your keratometer do not use a K index of 1.3375, then it is important to back calculate the K readings in a way that it match K index of 1.3375. This is because if the corneal readings are taken from a device which does not use K index of 1.3375, there could be a mismatch between the K index used by Keratometry device and IOL formula (in calculating net optical power of cornea) and therefore an error. To avoid this, Wolfgang Haigis (1) recommends the following:
1. Start out from radii of curvature or convert back from Ks to radii using the K index of the device.
2. Then reconvert to diopters from radius of curvature by using the K index (1.3375) which the IOL formula expects to have been used during keratometry.
In the below picture, in the IOL Master, you have an option to input the K index as default.
Most other optical biometry devices will have this option.
Since all IOL calculation formulae converts the anterior power curvature of cornea into net optical power of Cornea, care should be taken not to input net corneal power from a topographic device into IOL calculation formulae. If you want to utilize net corneal power that you have measured from the topographic device into IOL calculation formulae, a special formula like Barret Universal Toric Calculator formulae could be used where there is an option of entering your measured net corneal values. This is because the Barrett formulae in this case will not convert the anterior K values into net optical corneal power as in that case there will be a double correction.

The last but not the least important is to understand how does the modern optical devices measure the cornea ? The key here is to understand the Purkinje Reflexes from the cornea. None of these devices measure the Posterior Cornea ( with the exception of Zeiss Total Keratometry recently launched ). The IOL Master version V would throw six spots of light on the anterior cornea in a hexagonal pattern in the diameter of 2.5 mm. So the distance between each spot is 1.3 mm to the visual axis in a perfectly symmetrical and spherical cornea. The position of each spot reflecting back from the cornea and relative to the other light spots would be picked up and analyzed by the computer. Light reflections closer to each other would signify a steeper cornea and vice-versa.
The radius of curvature is determined by perpendicular imaginary lines that extend to the center of the cornea. If a cornea was absolutely spherical and a circle, only two spots of light would have been enough to determine the curvature. But a cornea is rarely spherical and has some amount of astigmatism in it. This therefore, demands more spots of light projected on the cornea. The lines that extends from the light spots on the cornea to the center of the circle helps us to determine the radius of curvature of the cornea in mm. As said earlier, this is converted back to diopter through the K Index and the formula D=n-1/r, where n is the K Index and r the radius of curvature..
Different Keratometers measure different diameter of rings of the cornea. That being said, more the device measures the central portion of the cornea, the more it may report a steeper cornea. This is because a cornea is generally prolate in shape and hence a steeper cornea is reported when a smaller diameter is measured.
However, the exception may be the VERION from Alcon. I have been often asked why the VERION reports a flatter cornea when it measures a very small central portion of the cornea.
My answer is that this is because the flattest portion of a hill is not in the middle but at its top. If you go beyond a certain area and measure too centrally, you may get more flatter cornea measured and reported than other devices. While this may be good for post myopic Lasik cases, this may not be very ideal for average patients, and even in eyes with central pathology. Keep in mind, the cone in a Keratoconus patient is not in the center, but inferiorly displaced or decentered (-Y axis ).
Lastly, I want to touch the concept of various K values in the form of TNP, TCRP, K1 &K2, SimK, IOL Master 700 TK, EKR, etc. With so many terminologies found in many devices it is often confusing to the user to understand the differences between them and use these values judiciously. Below are two short summaries showing the differences between the two. I hope you find it useful.


-----------------------------------------------------------------------------------------------------------------------
Reference:
https://www.myalcon-toriccalc.com/ (Alcon Toric calculator)
https://www.hoyatoric.com/ (HOYA Toric calculator)
Standardizing constant for ultrasonic biometry, keratometry and IOL power calculations, Jack Holladay JCRS vol 23, Nov 1997
*Development of the SRK/T intraocular lens impalnt power calculation formula, John A. Retzlaff, et al; JCRS Vol 16. May 1990



