Understanding Defocus Curve of multifocal IOLs
- Subhabrata Bhattacharya

- Jan 25, 2023
- 8 min read
Updated: Jan 19, 2024
When it comes to the field of Ophthalmology, understanding the science behind the product is as critical, as remembering the features, benefits and advantages of the product. Explaining the science, helps to create a ground for the surgeon to understand the value of the product in his/her practice. This science, may often be the road to create or address the ‘need’ that the product would address.
One such topic, is the science of Defocus Curve, and how the understanding of the science would help us to comfortably understand what the patients and clinicians can expect from the multifocal presbyopia correcting intra ocular lens(IOL). Thus we will look into the process of creating a defocus curve, its primary objective, and how one multifocal IOL can be differentiated from the other in terms of where will be the peak near focus, where will be the peak intermediate focus, and what will be the range of near and intermediate vision.
What we are trying to see ? - Objective of doing a defocus curve
At the outset, please remember, that the very objective of creating a defocus curve, is not to understand the vision that the patient is getting post operatively. The objective is to understand, what a multifocal lens is capable of giving to the patient, provided individual biometry, keratometry, and other variables are removed. In other words, we are looking to understand the lens function or lens capability of giving peak near and intermediate and its range of vision, than evaluating the patient post-surgery. Thus a Defocus Curve provides an opportunity to analyse the performance of presbyopia correcting IOLs by eliminating other influencing factors, and is not only helpful for clinicians but from a regulatory perspective also. Hence, the start of a defocus curve is to select a binocularly implanted multifocal patient, without any refractive surprise (6/6). If there is a pre existing refractive error, you should first correct the refractive error and make the patient 6/6 (BCDVA should be 6/6 as starting point of defocus curve). Ensuring the patient is 6/6 either uncorrected or best corrected removes biometry inaccuracies that may influence our understanding of what the multifocal presbyopia correcting IOL is capable to provide in terms of range of vision.
Understanding the basics:
Before we analyze the defocus curve in the figure 2 below, some basic concepts should be clear.
First, a convex lens converges rays of light. A convex lens is a plus glass that is being dialled in the phoropter. It is used to correct hyperopia to make rays of light fall on retina, as in hyperopia rays of light converge behind the retina.
Second, a concave lens diverge rays of light and therefore minus glass is dialed in the phoropter to correct myopia.
Third, diopter or the power of a glass is inversely related to its focal length ( Diopter=1/focal length) . 1 diopter of convex lens will have a focal length of 100 cms/1 m. Since the relation is inverse, a 2 diopter of convex lens will have a focal length of 50 cms. Thus higher the power of the glass, the focal length becomes smaller. A 4 diopter of lens will have a focal length of 100/4 or 25 cms.
Fourth, a concave lens, will make objects virtually come closer. That is why you dial a concave lens in a patient who suffer from near sightedness or myopia. Once concave lens of appropriate power is dialed, objects are brought closer, albeit virtually. That is the distance image that formed before the retina is brought on the retina by dialing the concave negative powered lens.

Fifth, in a monofocal lens there is only one focal point that would seat on the retina if there is no biometry error. In a multifocal IOL there is atleast another additional focal point . For a bifocal presbyopia correcting IOL like ReSTOR this additional focal point is the near focal point that seats before the retina (figure 1). As the patient looks at the near object, say reading a book, this near focal point seats on the retina while the distane focal point is pushed further away from the retina. Thus the patient reads the book with the help of the near focal point. As he/she looks further away at the distance, the near focal point recedes anterior to the retina and the distance will shift to the retina. The patient looks at the distance with the help of the distance focal point sitting on the retina. This is an over simplification of the process, but this would be sufficient to help us understand the Defocus Curve subsequently.
Sixth, a distance from 25 cms ( very close near work like sewing ) to 50 cms ( a distance were an average person would write) is our near vision. Generally an average person is comfortable to read at a distance of 38 to 45 cm from the eye, though a lot depends on the font size of the print, the height of the patient, etc. Intermediate distance refers to a distance from approximately 55 cm to 80 cm or more. A typical laptop work is done at a distance of 65 to 70 cm for most people.
So the question is what is the multifocal IOL in question capable of giving us at such distances from the eye?


Interpreting Defocus Curve:
Keep in mind the patient would all along and throughout the process look at the snellen chart.
You can see the x axis in Fig 2 is the lenses that we dial in. Remember these lenses signify the distance the patient is seeing the snellen chart from the eye. In this way a relationship can be derived between the lens vergence, and the distance acuity recorded. Such a graph enables us to understand what the lens is capable of at various distances from the eye. When no lens has been dialed in ( that is the patient is not de-focused) the patient is seeing 6/6 or 20/20 at a distance of 20 ft or 6 mt from the eye. This is our starting point.
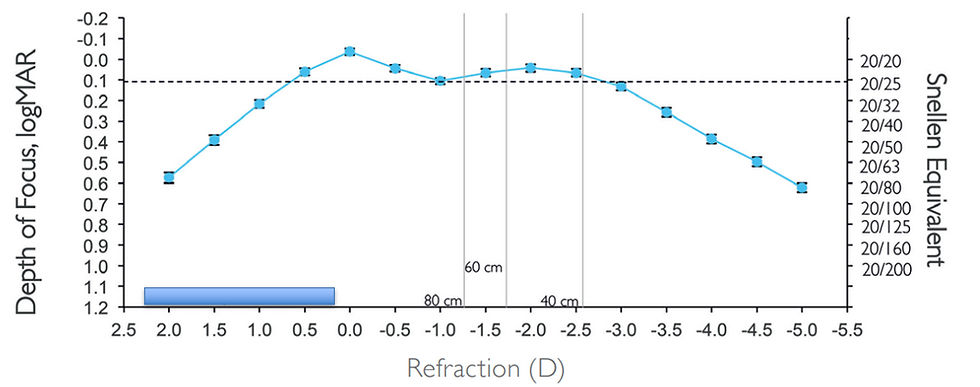
As we dial in the negative lenses, say -1 diopter lens, the snellen chart is virtually brought closer to the eye. Since a 1 dioptre of concave(negative) lens diverges and has a virtual focal point of 100 cms, the Snellen chart is as though brought 100 cms closer to the eye. At this point in a bifocal IOL you will note in the y axis the patient vision has dropped ( see figure 2). This is because neither the distance focal point, nor the near focal point are on the retina which is described in figure 4.

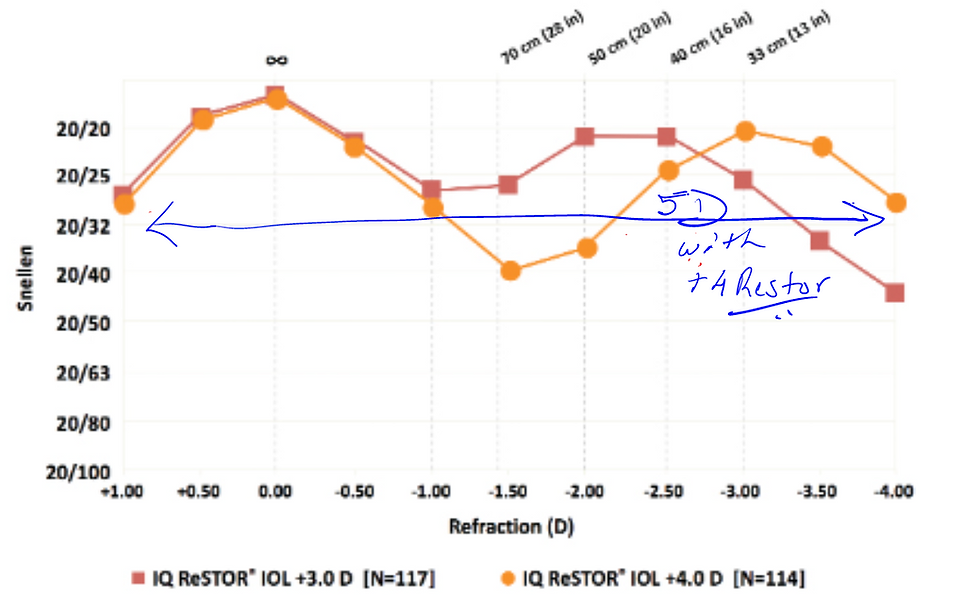
As you keep dialing more negative power lenses, the near focal point will keep going closer to the retina and the distance focal point is going to shift further away from the retina. Eventually, the patient's vision is going to jump to 6/6 as you dial the exact add power that is provided for the near reading in the multifocal IOL plane. That is, with Restor +3 bifocal IOL, the add power on the spectacle plane is 2.5 dioptre (3 diopter in IOL plane). When you dial a -2.5 dioptre lens the near focal point will shift to seat on the retina and the patient will see the Snellen chart again 6/6 with the near focal point now sitting on the retina (figure 2)
A 2.5 dioptre add power on the spectacle plane will mean a reading distance from the eye of 40 cm. If the patient reads 6/6 then it would mean the near vision with the Restor +3 will be at 40 cm.

Figure 6 is the defocus curve of a trifocal IOL. With a dialing of -1.5 glass that signifies a distance of 66 cm, the patient vision is 20/25. This is because a trifocal IOL has an additional focal point, the intermediate focal point. The defocus curve in Figure 2 of Panoptix IOL give an idea where the patient's peak intermediate vision will be - that is at a distance of 66 cm from eye the patient should get 20/25 or better.
How does the defocus curve help?
First, at its very basic the defocus curve in Figure 2 and Figure 6 helps us prove that this is not a monofocal IOL, but a bifocal and a trifocal IOL respectively. Otherwise how can you explain a patient reading the Snellen Chart with a -2.5 dioptre glass ? From a medico-legal perspective, this is a significant point.
Second, the defocus curves in figure 2 and figure 6 helps us to understand the functional vision amplitude/pseudoaccomodation that the patient is going to get for the respective IOLs. For example in figure 2, Restor +4 provides almost 5 dioptres of pseudoaccomodation that is better than 20/32 while the Restor +3 provides around 4 dioptres. See below the arrow mark depicting the pseudoaccomodation or functional vision amplitude with ReSTOR +4 (fig 7). You will have what your multifocal IOL
Third, as discussed at the outset the defocus curve gives us an idea what would be the range of near and intermediate distance that the patient will be getting from these lenses and at what distance from eye the near and intermediate will be at its peak. This helps clinicians an uniformed choice of the multifocal IOL based on patient lifestyle and need.
Fourth, the defocus curve can help the clinician to make a choice between two or more multifocal IOLs based on the patient's need.
Defocus curve limitations
There is no standardization in methods of generating defocus curve in the industry. Multiple factors can still influence defocus curve like pupil size, induced astigmatism, chart distances, etc. Several studies have shown that diffractive, or diffractive -refractive multifocal IOLs are influenced by patient's pupil size. My favourite study is a more than decade old study by Alfonso et al (Corelation of pupil size with visual acuity and contrast sensitivity after implantation of an apodized diffractive intra ocular lens JCRS 33;430-438; 2007) that showed Restor +4 (SN6AD3) had better distance VA with a large pupil size but worst near VA. Therefore when you look at the defocus curve and compare between two different multifocal IOLS, do question what was the pupil size of the patients with which the defocus curve was generated.
Patient contrast effects defocus curve outcomes too with reduced contrast levels may be associated with reduced VA across a range of distance. Thus while comparing defocus curves of two multifocal IOLs, it would be necessary to understand if similar contrast levels/light conditions have been used.
When comparing two multifocal IOLs on the basis of defocus curve, care must be taken to see if both group of patients had similar residual astigmatism levels. If patients have residual astigmatism, this will effect the defocus curve. It is important that in such cases the patients are made BCDVA 6/6 or 0.0 logmar (this has been explained at the outset).
Viewing chart distances are not always standardized. Even if care is taken to standardize the viewing distance, that is 20 feet or 6 meters is actually so, we have to remember that any object that is less than infinity will have negative vergence. Thus negative vergence at distances less than infinity has to be adjusted for. Light coming to eye from a distance of 4 m will have a negative vergence of -.25D that needs to be adjusted for. Therefore dialing a -2.0 dioptre glass in the spectacle plane will not equate to 50 cms, but 45 cms as negative vergence of -.25D has to be accounted for.
By this arguement a defocus curve tested at 6 mts will have less negative vergence discrepancy than if performed at 4 m. Thus direct comparison of defocus curve of one multifocal IOL may not be possible with another if they are from two different chart viewing distances.
By this arguement a defocus curve tested at 6 mts will have less negative vergence discrepancy than if performed at 4 m
As a clinician or industry professional what do I need to ask when I see a defocus curve?
If I have to compare between two multifocal IOLs I need to consider the following :
What was the UCDVA (un corrected distance visual acuity) of both group of patients?
What was the BCDVA (best corrected distance visual acuity) of both group of patients
What is the post operative ACD (ELP) and average AL and K readings of both group of patients. ( To see how these matters do consider reading Mystery of the Near with Presbyopia Correcting IOLs by clicking on the link https://www.quickguide.org/post/problem-with-near-vision )
Is the pupil size considered and same for both group of patients
At what distance is the defocus measured and plotted? ( a -.25d to be dialled for 4m charts)
Conclusion
Despite the above challenges, defocus curve remains one of the most important ways of understanding lens capabilities in an objective way. While modular transfer function (MTF) helps us to understand the optical properties of the lens in terms of image quality and contrast (discusssed in detail https://www.quickguide.org/post/modulation-transfer-function-mtf ) defoucs curve helps industry professionals and clinicians understand the lens capabilities and what the patient can expect to get in terms of near and intermediate.





